Six Effective Strategies to Alleviate Plantar Fascia Pain 
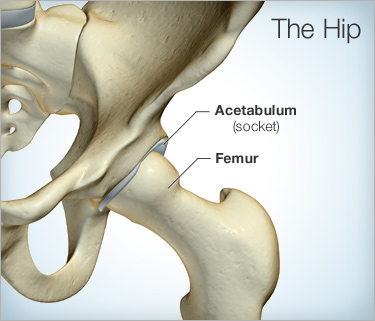
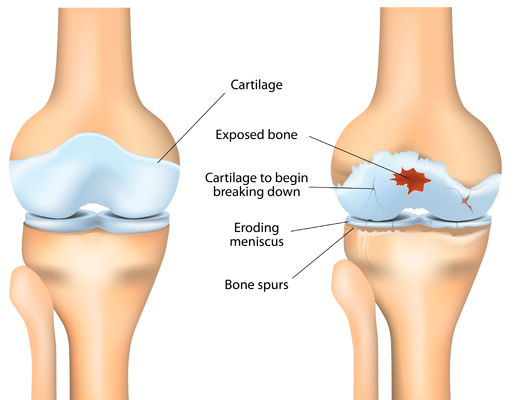
Plantar fasciitis is a common condition characterised by pain and inflammation of the plantar fascia, the thick band of tissue that runs across the bottom of your foot. It can be a debilitating condition, impacting daily activities and causing discomfort with every step. However, with the right approach, it is possible to manage and alleviate plantar fascia pain effectively. As a physiotherapist, I’ve encountered many cases of plantar fasciitis, and I’ve compiled a list of six top strategies to help you find relief and get back on your feet.
- Stretching Exercises:Stretching is crucial for relieving tension and tightness in the plantar fascia and surrounding muscles. Simple exercises like calf stretches, toe stretches, and plantar fascia stretches can help improve flexibility and reduce pain. These stretches should be performed regularly, ideally multiple times a day, to maintain flexibility and prevent further stiffness.
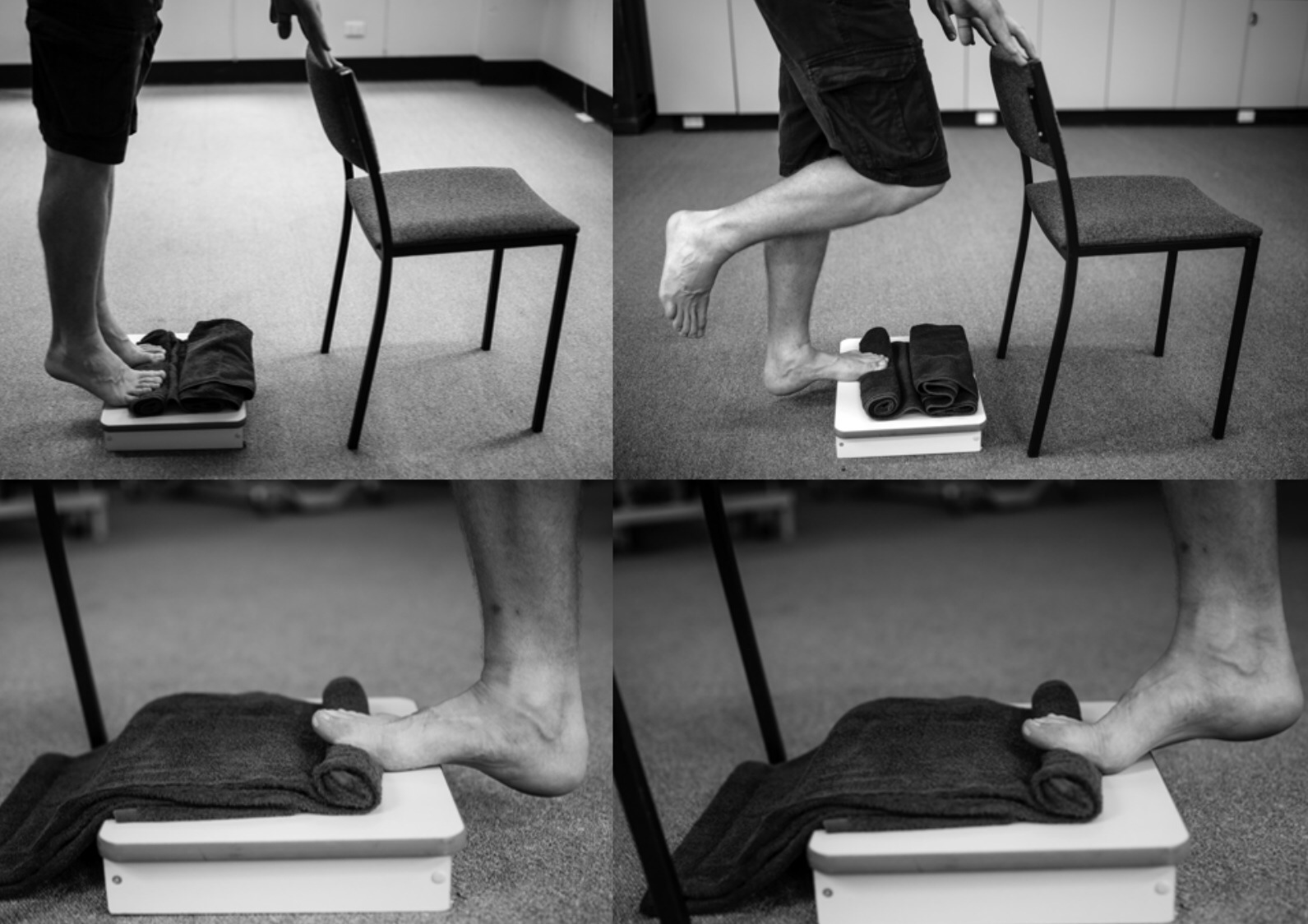
- Strengthening Exercises: Strengthening exercises focus on improving the strength and stability of the muscles in the feet and lower legs, which can help support the arch of the foot and reduce strain on the plantar fascia. Exercises such as toe curls, calf raises, and towel scrunches can be effective in building strength and resilience. Gradually increasing the intensity and frequency of these exercises over time can lead to significant improvements in pain and function. We recommend using a fasciitis fighter (pictured below) to incrementally load the plantar fascia tissue.
- Proper Footwear: Supportive shoes with good arch support and cushioning can help alleviate pressure on the plantar fascia and provide stability during walking and other activities. Avoid flat shoes or high heels, as they can exacerbate symptoms and increase the risk of injury. Consider using orthotic inserts or custom-made shoe inserts for additional support and comfort.
- Ice Therapy: Ice therapy is an effective way to relieve pain associated with plantar fasciitis. Applying an ice pack to the affected area for 15-20 minutes several times a day can help numb the pain. It’s important to use a barrier such as a towel between the ice pack and the skin to prevent ice burns. Additionally, rolling a frozen water bottle under the foot can provide targeted massage and cooling therapy.
- Massage and Foam Rolling: Massage therapy and foam rolling can help alleviate tension and tightness in the muscles of the foot and lower leg. Techniques such as self-massage with a tennis ball or foam roller can target trigger points and release knots in the plantar fascia and surrounding tissues.
- Rest and Recovery: Finally, allowing adequate rest and recovery is essential for healing and preventing further aggravation of plantar fasciitis. Avoid high-impact activities that put excessive strain on the feet, such as running or jumping, until symptoms improve. Instead, opt for low-impact exercises like swimming or cycling to maintain fitness without exacerbating pain. Adequate rest combined with the aforementioned strategies can expedite the healing process and prevent recurrence of plantar fasciitis.
Plantar fasciitis can be a challenging condition to manage, but with the right approach and consistency, it is possible to find relief and regain function. By incorporating stretching and strengthening exercises, wearing supportive footwear, using ice therapy, practicing massage and foam rolling, and allowing adequate rest and recovery, you can effectively alleviate plantar fascia pain and get back to enjoying your daily activities pain-free. As always, if you’re experiencing persistent or severe pain, consult with a physiotherapist or healthcare professional for personalized treatment and guidance.