Shoulder pain is a common problem that affects people in all walks of life.
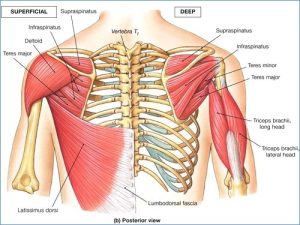
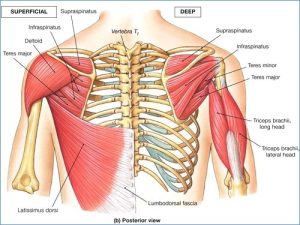
Everyone has heard about the rotator cuff BUT what does it do and where is it?
The rotator cuff is a group of 4 muscles that reside on the shoulder blade and attach onto the top of the arm bone. Their primary job is for stabilising and controlling the arm bone within the socket.
Shoulder pain can manifest in a variety of ways. From insidious onset over time, a large disruption to the shoulder following trauma, overuse injuries or instability after a dislocation. A large proportion of people attend our physio clinic with no idea of how their shoulder pain started and it gradually worsens over time. I tend to triage a shoulder injuries into 3 distinct areas in which, each treatment will differ drastically
The Three Buckets
The Stiff + Painful Shoulder
These shoulders lack sufficient range of motion to move appropriately causing pain and dysfunction.
It is associated with a hitching pattern in which, the shoulder cannot reach full range of motion when lifting to the front, the side and behind the back. It typically effects shoulders of the older demographic with osteoarthritis or post trauma. Frozen shoulder can create a stiff and painful shoulder, this generally affects the 40-60 year old demographic, mostly females.
What to look out for:
- Pain whilst doing you bra up or reaching behind your back.
- Difficulty reaching across your body to wash the opposite shoulder.
- Movement restriction even when arm is supported.
- Night pain lying on the affected shoulder.
- A deep clunk sensation is a sign of an osteoarthritic shoulder.
- Bunching of the shoulder as you lift it up in front.
The Wobbly Shoulder
These shoulders lack the appropriate neuromuscular control to keep the shoulder joint centred in the socket. This will affect the younger population between 18-25 years old. They’re more likely to dislocate their shoulder during sport. People with hyper-mobility is another cause for the wobbly shoulder, so if you’re naturally a bendy person then your more likely to fall into this bucket.
What to look out for:
- No restriction in movement.
- Clicky feeling in the shoulder upon movement.
- Perhaps a vague nerve sensation down your outer upper arm when playing contact sports.
- Pain throughout the extremes of movement and a feeling of ‘looseness’.
The Weak + Painful Shoulder
General weak shoulder stabilisers/muscles that create pain and dysfunction associated with upper body exertion. These shoulders tend to lie in the 30-60 year old demographic and it is the inability for the shoulder to keep up with the what you are asking it to do and therefore gets sore. It is associated with a shoulder that can move relatively well but gets ‘catchy’ throughout the movement. This shoulder will probably hurt after the gym if you’re training and perhaps give you a fair bit of grief at night time when you lie on that side. There is generally focal tenderness on the outer aspect of the arm that may radiate into the upper arm and is associated with either acute or chronic rotator cuff tendon tearing.
What to look out for:
- Painful at night lying on affected side.
- A painful arc when lifting the arm to the side, meaning there is a period of pain when you lift up to the side that generally subsides by the time you reach the top.
- Difficulty lifting arm up to the side without pain or catching
- Pain after activity or exertion generally 24-48 hours after.
- Intermittent pain over upper outer arm.
- Insidious onset with no direct mechanism of injury.
- Very rarely do these shoulders hurt when you’re not using them.
Can you figure out which bucket your shoulder fits into?
Can Physio help or do I need surgery?
Each shoulder needs to be assessed individually and then triaged into what bucket the shoulder fits into. Taking into account age, gender, activity levels, patient symptoms, goals and general conditioning the management will change according to the patient. For example: A 30 year old male with a rotator cuff injury from bench pressing cannot be rehabbed the same as 50 year old women with a stiffening shoulder.
The premise is to find YOUR deficit and restore THAT deficit in line with what goals you have.
- Restoration of joint range through manual therapy and a mobility plan.
- Improve shoulder neuromuscular control and joint stability with rotator cuff activation exercises and stabilisation drills.
- Improve shoulder rotator cuff strength in a isolated fashion then progress to global conditioning.
- Referral on if indicated to a surgeon: This occurs when there is trauma, gross loss of strength, copious amounts of pain, large amount of shoulder dysfunction and an abundance of night pain.
- Ultrasounds and MRI scans are hit and miss – There is a place for imaging a shoulder when indicated. But there is a very low correlation for imaging and shoulder pain. Meaning what we see on an MRI may have everything to do with why your shoulder hurts, but a large percentage has nothing to do with why your shoulder hurts.
What we hear all the time is “How is Physio going to help if I have torn rotator cuff?”
What we do know is most people over the age of 30 in non-symptomatic shoulders will show a raft of changes on an MRI including rotator cuff partial/full thickness tears and bursitis so take your scan with a grain of salt and get on with your rehab if you want results 🙂
If you need any help with your shoulder rehabilitation come see us at The Physio Depot!
Written by Patrick Lincoln
(Physiotherapist)